Many veterans of the biologics industry presume that emerging therapeutics such as cell and gene therapies (CGTs) require production facilities that differ substantially from those for monoclonal antibodies (MAbs) and other conventional biologics. But experience with designing CGT facilities bears out that far more synergies than differences exist across facilities for conventional and advanced therapies. Herein, I call attention to some of those shared design concerns and demystify facilities and engineering requirements for CGTs.
Many veterans of the biologics industry presume that emerging therapeutics such as cell and gene therapies (CGTs) require production facilities that differ substantially from those for monoclonal antibodies (MAbs) and other conventional biologics. But experience with designing CGT facilities bears out that far more synergies than differences exist across facilities for conventional and advanced therapies. Herein, I call attention to some of those shared design concerns and demystify facilities and engineering requirements for CGTs.
Observing the Synergies
Many processes have evolved from adherent-based cell lines and processes, and although some commercial processes still use those platforms, most now operate as suspension platforms with scalability and operational advantages. Gradually, viral-vector gene therapy processes have transformed so that they can produce at scales on par with small-scale MAb facilities. Of course, the clearest difference between production of gene therapies and MAbs is that the former requires viral vectors, which entail additional steps for transfection. Otherwise, unit operations are similar for production of gene therapies and conventional biologics, including steps for development of master and working cell banks (MCBs, WCBs), inoculum preparation, and cell culture, followed by numerous harvest recovery and purification steps. Today, a 500-L or 1,000-L gene-therapy operation wouldn’t look substantially different from a small-scale MAb facility.
Working with viral vectors certainly increases a facility’s biosafety level (BSL) requirements. Such facilities must incorporate adequate heating, ventilation, and air conditioning (HVAC) systems and containment strategies such as positive- and negative-pressure airlocks for entry into and exit from production suites. For instance, handling of viral vectors requires a negatively pressurized suite and perhaps once-through airflow to minimize contamination risks in the event of viral exposure. But all told, processes that use adenoassociated virus (AAV) or lentivirus (LV) — which are the most common vectors for gene therapies and gene-modified cell therapies — must operate within BSL-2 environments. Such requirements aren’t terribly onerous.
Other parallels abound. The MAb industry still talks frequently about transitioning to ballroom and dance-floor designs, and similar conversations are occurring regarding CGT facility design. But companies across modalities remain slow to adopt ballroom layouts. My organization, DPS Group, observes that biopharmaceutical companies still are committed to designing facilities with dedicated areas for upstream, downstream, and viral-vector operations. And we still are not witnessing companies take the big leap into ballroom setups for viral-vector gene-therapy facilities.
Toward Closed Processing
Thinking back to 2017, when DPS Group began designing facilities for autologous products, specifically gene-modified cell therapies, I recall planning for numerous small-unit operations. My group observed preferences for dedicating grade B cleanrooms to each patient batch, with cell processing performed in grade A biosafety cabinets. Companies now are transitioning to closed processing.
Currently, we are involved in designing what will be one of Europe’s largest facilities for chimeric antigen receptor (CAR) T-cell therapies. All unit operations in that facility will use closed processing. Thus, they can be conducted in grade C cleanrooms. The facility still will require the additional security afforded by biosafety cabinets and laminar airflow units for some activities. Such commercial facilities are being designed to produce thousands of patient batches per year.
In CAR-T processing facilities, we still are dealing with individual patient batches. Although designing for 2,000 batches per year equates to only a few batches per day, those units need to be scheduled according to patient need. Thus, facility design still must consider multiple scheduling scenarios. But in large patient-batch facilities, multiple batches now can be processed in one area at a time, with appropriate controls. Such a setup is substantially different from what my group observed even four years ago. Closed processing enables handling of multiple batches in the same area so long as your segregation strategy is sound and sufficiently assessed for risk.
Such facilities can be designed to prevent mix-ups. We apply discrete event simulation (DES) software for “soft” modeling. DES tools can provide almost minute-by-minute mapping of a facility’s equipment utilization and materials and personnel flows.
The main purpose of a model is to ensure that all functional areas are sized appropriately. That helps to optimize placement of equipment units and manufacturing operators. Because CAR-T facilities work with patient cells, which can be compromised from previous cancer treatments, cell growth profiles can differ significantly across apheresate lots, resulting in a range of batch durations. Cell expansion steps can take from five days to 15 days to achieve required cell densities. Thus, the number of process-equipment units in a facility must be modeled statistically based on probabilities of when samples might arrive and how long cell expansion could take for each patient.
DES software also can visualize how multiple batches move in tandem to ensure no crossover of materials. In principle, several cell-processing unit operations representing multiple patient batches can operate within a given suite (provided that we are dealing with a single viral vector).

Figure 1: Integrated sampling pouches are removed by disconnection through sterile welding to maintain a closed environment within Miltenyi Biotec’s CliniMACS Prodigy system. (https://www.miltenyibiotec.com)
Technologies for closed processing continue to evolve, and several vendors are leading in this area. Miltenyi Biotec, Cytiva, and Terumo BCT are among the most advanced suppliers in terms of closed, semiautomated processing (Figure 1). All those companies have closed individual process-unit operations, with developments underway to create a closed, end-to-end process. Despite significant improvements in closed-processing equipment, many CGT developers are waiting expectantly for advancement in automation to facilitate end-to-end processes. Such developments will require engagement among manufacturing organizations, equipment vendors, and technology developers.
Regulatory expectations can complicate the facility-design calculus. DPS Group recently helped to design a facility in Europe for an autologous CAR-T process that was being transferred from an American site. During the project’s feasibility stage, we leveraged data from another approved EU CAR-T processing facility with which our team had worked. That put a low limit on the number of patient batches that would be processed per suite. A low number was used in response to a challenge on the previous project from the local regulatory agency. However, based on some design improvements for our new facility — with closed process steps operating in grade C cleanrooms, and with robust management of chain of identity (CoI), batch-segregation control, and track-and-trace protocols — we ultimately were permitted to increase the number of patient batches per suite to three times that allowed in the older facility. This example demonstrates just how quickly the process of CGT design is evolving.
All told, closed processing does not permit a facility-design free-for-all. The number of batches that can be handled simultaneously will differ by product type, process design, and jurisdiction.
Seldom-Considered Risks
Facility design requires thorough understanding of how a process needs to work. Design teams must account for all adjacencies. They need to know that an operation will move logically through a facility with minimal potential for product mix-ups and contamination events. Thus, much effort goes into consideration of material and personnel flows.
Retrofit or Build Anew? Today, facility designs for CGT operations usually incorporate proprietary modular cleanroom systems. Cleanrooms don’t need to be “podular” as such. Many modular designs include wall and ceiling systems with flush-fitting panels. Such materials become fixed in place upon assembly but can be easy to dissemble. They also are designed to handle considerable cleaning and disinfection.
From a design perspective, retrofitting legacy facilities and establishing new ones entail similar planning. Retrofitting still requires that you rip out existing materials and then recreate your cleanroom environments using proprietary panel systems and new HVAC systems. From participating in many such projects, my group has noticed that retrofit requests tend to come for early phase clinical facilities. On the other hand, commercial-scale operations primarily request designs for new, fit-for-purpose facilities.
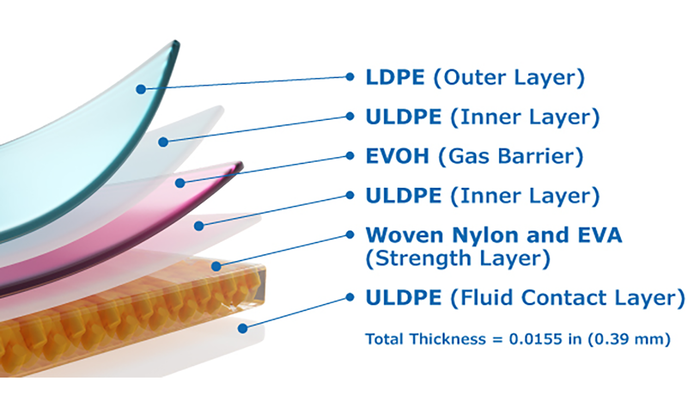
Single Use and Biosafety: SU systems can pose unexpected problems for retrofitted facilities. CGT operations consume tremendous amounts of SU bag systems, tubing sets, and filter trains, all of which must be “kitted” in an appropriate area and then brought into grade C or B cleanrooms. Kits usually are prepared in grade C environments, and some of those kits might need to transfer into grade B areas. But moving them without adequate wipe-downs and decontamination can generate environmental excursions. When prepared in grade C zones, kits must be boxed carefully under laminar airflow, and great attention must be paid to spaces for kit decontamination. Such considerations are critical during facility design yet rarely receive attention until problems arise.
Knowledge of such complications comes from experience. A DPS team is involved in the startup of a facility for a commercially available, allogeneic stem-cell therapy. The operation is being transferred from another manufacturing center. The new site is a direct technology transfer from the donor site, so all bioprocessing is performed inside grade A biosafety cabinets within grade B rooms. During the facility startup, much consideration had to be given to the protocol for moving kits in and out of grade B rooms without preventing environmental excursions. A future phase is likely to have some design modifications, all part of learning by experience and designing more effectively for the next generation.
Conditions are evolving in that facility. To ensure decontamination of materials brought into grade B environments, the team is exploring UV airlocks and even vaporized hydrogen peroxide (VHP) transfer isolator modules for aseptic delivery. A subsequent phase of this project will move remaining open process steps into isolators in grade C cleanrooms; performing manual activities in a cabinet within a grade B cleanroom poses product risks. Again, such concerns are important but generally do not receive attention until facility qualification. Proactive facility design is imperative.
Although CGT facility designs must account for several risks, a primary consideration is that such drug products cannot undergo final sterile filtration. Engineers must rely on design elements, process equipment, and cleanroom integrity to ensure product sterility. That factor explains, in part, why CGT companies — especially those producing cell therapies — are moving toward closed processing in grade C cleanrooms. Likewise, regulators are pressuring fill–finish facilities to adopt isolator technologies, which provide the highest level of protection for CGT products.
What to Do with Waste? Management of plastic waste, especially that contaminated by viral vectors, must be addressed differently for each facility. Some CGT companies prefer to build onsite decontamination capabilities; others bag everything and move waste offsite for decontamination. Regardless of preference, disposal must be examined. In-house waste management requires special decontamination areas that house large-chamber autoclaves. Even if waste travels offsite for decontamination, flowpaths with segregated two-way staging areas need to be established. Thus, CGT facility design must account not only for incoming materials and outgoing products, but also for movement of waste out of production suites.
Some companies understand the flows of materials, personnel, products, and waste more completely than others do. My group’s site in Boston, MA, often works with Cambridge-based startups. Many such companies need guidance because their processes previously operated at laboratory scales and did not necessarily follow current good manufacturing practice (CGMP). We work closely with CGT newcomers to determine the best workflows.
Large organizations such as the CAR-T developer that I noted above already have constructed facilities for similar products. Such companies can leverage past and current experiences. But even with large organizations, we still challenge design assumptions to identify risks and make changes. Changes are made to each project, and factors that should have been considered at the outset but were not can be implemented during future design phases or into future projects.
Regulatory Nuances: CGT facility design requires careful reckoning of regulatory standards. Consider HVAC systems, which typically are classified as ISO-7 or ISO-8 systems according to International Organization for Standardization (ISO) schemes and as grade D, C, and B systems according to EU GMP standards. In some cases, an ISO classification does not translate directly to a particular grade in Europe. EU GMP standards can be more onerous than their American counterparts. For example, if an HVAC system has operated under ISO-8 in the United States, transferring it to a grade D cleanroom environment might not be acceptable in Europe. EU regulators might prefer operation in a grade C area.
Tools for Risk Assessment
Facility design projects typically follow a “stage-gate process” that begins with a high-level feasibility study and moves into incrementally more-detailed planning. The design-concept phase still examines facility plans from a high level, visualizing bioprocess workflows rather than drawing out piping and instrumentation diagrams (P&IDs). Concept design enables capital estimates within a ±20% margin of error, whereas estimates made during subsequent stages can come within a ±10% margin of error.
We usually approach regulatory agencies in the design-concept phase to talk through what our process flows look like, where processing will be open and closed, where we will enact containment and airlocking strategies, and so on. We critique all those considerations early so that we know — while the design is still on paper — that a project is going in the right direction. Sometimes regulators will find areas of concern or identify process flows that require improvement.
Although risk assessment can be performed using failure modes and effects analysis (FMEA), my group applies a CGMP template that asks detailed questions about every aspect of a process, covering how material is handled from the moment that it arrives in the facility to when a finished drug product leaves. This review accounts for handling of individual starting/raw materials, design attributes, and control strategies for processing, data acquisition, and analytics.
Process Modeling: DES software facilitates process modeling for autologous cell therapy facilities because it is well suited to the intricacies surrounding handling of multiple single-patient batches. For viral-vectored gene therapies, we use other modeling tools that emphasize equipment sizing and occupancy. Intelligen’s SuperPro Designer and SchedulePro software packages can be powerful tools for mapping out process flows, evaluating mass balances, sizing equipment and utilities, and identifying process and equipment redundancies.
Facilities for autologous cell and gene therapy products tend to be utility light. They operate at small scales within small unit operations. Thus, such facilities usually do not use skids that hook into utilities for supplies such as clean-in-place (CIP) fluids. But SuperPro Designer and SchedulePro software packages are valuable for modeling viral-vector and gene-therapy facilities that operate at large scales (1,000–2,000 L) and that require broader utility access.

Figure 2: Aseptic Technologies’ Crystal M1 filling station is designed to meet small-scale, current good manufacturing practice (CGMP)-compliant pharmaceutical filling needs. (https://www.aseptictech.com)
Sterile Filling for Small Volumes
Optimizing Small-Scale Filling: Design considerations for CGT sterile-filling operations can be challenging. The number of vials or bags that can be filled will differ significantly across products and processes. For instance, because CAR-T operations tend to generate one batch per patient, they deliver relatively few drug products. But how do you perform sterile filling for small quantities cost-effectively and without risking product losses within a filling mechanism? Until now, standard practice has been to fill manually within biosafety cabinets housed in grade B environments, but regulators worry about such measures. Reviewers will expect filling to occur in isolators and with minimal manual operation.
New equipment designs are proving to be quite adept at handling small-volume fills for low product numbers. For instance, the Crystal M1 filling station (Aseptic Technologies) provides a robotic, CGMP-compliant solution that can be installed within a biosafety cabinet or isolator (Figure 2).
Viral-vector and gene-therapy facilities that operate suspension-based processes at 500 L, 1,000 L, or even larger scales might need modular robotic filling units within isolators. One such technology is the SA25 Aseptic Filling Workcell system (Vanrx Pharmasystems, now part of Cytiva). Small-scale robotic filling technologies now are entering the mainstream. That development could prove useful in the CGT industry.
GMP Readiness: Challenges are likely to arise with regulating emerging filling units. In 2017, for instance, DPS led an expert-team review of Vanrx’s workcell technology. We were challenged when reviewers observed that the isolator lacked ports. How, then, could the manufacturer install settle plates to conduct environmental monitoring? As with all new equipment, however, risk assessment is paramount. Since that review, the technology has been approved for use in some jurisdictions.
Such problems crop up, in part, because new filling solutions are trying to keep pace with the CGTs on which they are developed. Commercialization timelines are much faster for CGTs than for traditional biologics, and CGT developers often believe that the lowest-risk approach is to continue with technologies and processes that they have used during research and development (R&D) phases. Sometimes that equipment just isn’t ready for GMP manufacturing, but CGT developers are reluctant to change anything because they want to get to market quickly.
The unpreparedness of many small-scale filling solutions for GMP manufacture helps to explain why many CGT companies resort to open processing. However, equipment vendors are working closely with CGT companies on their commercialization journeys. One of my current clients is a European startup that has developed an innovative cell therapy. The company wants to establish an end-to-end process. One equipment vendor that has consulted with my client seems to be ahead of other suppliers in terms of end-to-end processing, but the client’s R&D team used a different vendor to develop its therapy. Ultimately, the client chose to work closely with its original vendor to close that process and come up with an end-to end solution.
That example serves to show that collaboration between CGT developers and technology suppliers will be critical to manufacturing and commercial success. Such partnerships are happening already, and process improvements are developing rapidly in turn. Ultimately, equipment vendors will play a large part in advancing end-to-end CGT solutions.
Suppliers also are exhibiting greater understanding of regulatory concerns than they have in the past. These companies are considering regulatory processes alongside expectations for development and improvement. Regulators are displaying greater acceptance of process innovations, with an appreciation that even though a new technology may not be perfect in the first generation, its advances on the previous status quo outweigh disadvantages so long as risks can be managed to ensure patient safety while a new, second-generation model or technology is developing. Patient safety is paramount. Improvements will come in time.
Areas of Continuing Need
Closed, automated, end-to-end processing is the Holy Grail of biopharmaceutical facility design — and we are close to realizing that prospect. For cell therapy and gene-modified cell therapy processes, companies such as Miltenyi are working on potentially game-changing solutions. End-to-end processing would enable CGT manufacturing to fit comfortably within a ballroom configuration. Automation not only would minimize risks from manual interventions, but also would help companies realize significant savings for cost of goods (CoG) and labor.
Scalability remains a CGT pain point, though, particularly for cell therapies. CAR-T processing facilities currently can scale out but not up. Although closed, end-to-end processing represents an ideal solution, innovative solutions for stacking processing units can help for the meantime to mitigate associated design challenges. The Cocoon cell-therapy production system (Octane Biotech, part of Lonza Pharma & Biotech) is potentially a significant achievement in that regard. Still, the cell therapy industry needs options to help it scale up rather than out. Improved scalability will enable design of neater, more space-efficient facilities than are currently possible.
Acknowledgments
BPI thanks editorial advisor William Whitford for his feedback on this article and for valuable advice on the topic of facility design for cell and gene therapies.
Sue Cooke is head of the Strategic Consulting Group at DPS Group Global, Unit 3096-3098, Lake Drive, Citywest Business Campus, Dublin 24, D24 E1CY, Ireland; 353-1-466-1700; https://www.dpsgroupglobal.com.