Vertex ‘hitting the ground running’ with Casgevy launch
Vertex says physicians prefer prescribing gene edited therapies to other gene therapy mechanisms as it rolls out sickle cell disease treatment Casgevy (exa-cel).
In December, Vertex Pharmaceuticals and partner CRISPR Therapeutics won approval from the US Food and Drug Administration (FDA) for sickle cell disease and transfusion-dependent beta thalassemia (TDT) treatment Casgevy. Weeks prior, the UK’s Medicines and Healthcare products Regulatory Agency (MHRA) made history by approving Casgevy as the world’s first CRISPR-based gene-edited therapy.
As such, Casgevy’s launch was the hot topic of discussion during Vertex’s presentation at the JP Morgan Healthcare Conference this week, with CEO Reshma Kewalramani describing the therapy as “an enormous opportunity to serve patients” with a “multibillion dollar market potential.”
There are potentially 35,000 patients in the US and Europe, and while there will be competition from bluebird bio’s Lyfgenia (lovotibeglogene autotemcel) – also approved in December to treat sickle cell disease – she told investors Vertex has “hit the ground running” in rolling out Casgevy.
“We know that the patients can be served with the approximately 50 authorized treatment centers we are planning in the US and the approximately 25 treatment centers we are planning in the EU,” she said, adding nine centers are already activated in the US and three are already activated in the EU.
And with regards to access and reimbursement in the US, Kewalramani cited the recent agreement with Synergy, a healthcare payer covering approximately 100 million patients commercially. “While we continue to secure coverage and additional providers above and beyond Synergy, for now people in the US can access Casgevy through single agreements, and in the EU can access Casgevy with the potential of early access programs.”
The patient’s journey:“First, pretreatment. Initially, when a potential exa-cel patient and their hematologist decide the therapy is right for them, the patient is then referred to a transplant physician at an ATC [Authorized Treatment Center]. Once that referral is scheduled, the patient then undergoes a full workup to determine whether they are fit for treatment with exa-cel,” Vertex COO Stuart Arbuckle said in November. “Second, cell collection and manufacturing. This phase involves mobilization to move the blood stem cells from the bone marrow into the peripheral blood, where the cells can be collected through apheresis. The patient’s cells are then sent to our manufacturing facilities, where they are edited and then tested for quality control. Cell collection takes longer for sickle cell disease patients given the need for two months of red blood cell transfusions prior to mobilization and on average two rounds of mobilization and apheresis. In contrast TDT patients do not require premobilization transfusions and typically only require one round of mobilization and apheresis.” The final phase, is treatment. “Once the edited cells are ready, the patient starts the treatment phase, which includes myeloablative conditioning, infusion of the edited cells, at which point we will recognize revenue for the therapy, and then waiting for engraftment and post-infusion care. A critical timing factor in this phase is the patient’s preferred timing for treatment, as they must choose a time that works best for their lives, given that this step involves an approximate one-month hospital stay.” | |
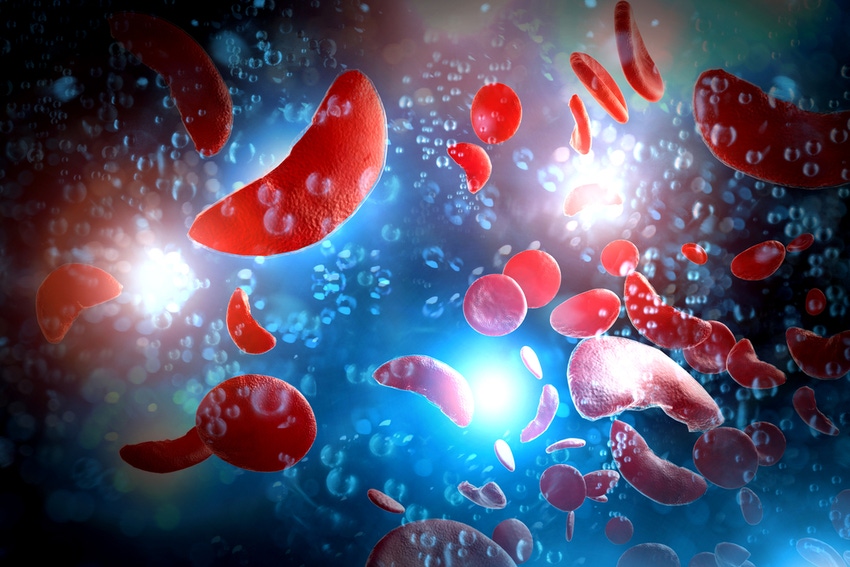
Casgevy is an autologous, ex vivo CRISPR/Cas9 gene-edited therapy in which a patient’s hematopoietic stem cells are edited to produce high levels of fetal hemoglobin (HbF; hemoglobin F) in red blood cells. HbF is a form of the oxygen-carrying hemoglobin that is naturally present at birth, which then switches to the adult form of hemoglobin.
The nature of the modality is a key differentiator in Casgevy’s potential success, she said, citing market research that found “physicians prefer gene editing therapy to gene therapy.”
When asked why, she spoke of the understanding of the difference between gene editing and gene therapy. “There is awareness that by mechanism-of-action, there is the possibility for random insertional mutagenesis with a gene therapy approach that uses a viral delivery mechanism. And there is awareness of the safety and efficacy data before the approval based on the New England Journal of Medicine papers and presentations at ASH, etc, for what the benefit risk and the efficacy is. And I expect that that is the reason there is this preference for gene editing.”
About the Author(s)
You May Also Like







