Are You Ready for a Tech Transfer? Part 1: Challenges and Critical Factors for Success in Cell Therapy Development
https://bioprocessintl.com/wp-content/uploads/2015/04/McIntyreSuman-VV-FINAL1.mp3
Technology transfer moves a process into a different environment and as a result, the
product should be properly defined before the transfer is initiated. Before technology transfer, raw
biological material collection (e.g., bone marrow, apheresis) and manufacture may be colocated,
typically at a clinical site (a). Following technology transfer, clinical and manufacturing sites are no
longer in close proximity (b).
Cell therapies offer enormous promise for treatment of a range of conditions by replacing damaged tissue or leveraging the body’s own resources to heal itself. Not surprisingly, the cell therapy industry is growing rapidly and is poised to have a major impact on healthcare and disease treatment. The Alliance for Regenerative Medicine (ARM) has reported on the robust state of the industry, noting that revenue from cell-derived products grew from US$460 million in 2010 to $1.3 billion in 2013 (1).
A critical aspect of cell therapy development is transfer of knowledge from a development organization to a manufacturing organization. The development organization (product sponsor) is generally the transferring site. A contract manufacturing or contract development and manufacturing organization (CMO or CDMO, respectively) often is the receiving site. In general, technology transfer to a CDMO is advised when a sponsor company requires the resources, capacity, facilities, and/or expertise directly relevant to cell therapy to meet industrial and regulatory requirements needed to advance a therapeutic product toward commercialization. So it is essential for a sponsor company to evaluate the strategy, timelines, and infrastructure necessary for a successful and streamlined technology transfer. In one sense, a rapid transition to good manufacturing practice (GMP) manufacturing at the receiving site may seem like an obvious goal. But in practice, such reckless speed can lead to an incomplete transfer or an unstable process and/or analytical methods. Consequently, that can lead to unnecessary deviations and additional time and resources required to overcome them.
Key factors in technology transfer include having a dedicated and multidisciplinary team, an attention to detail, a focus on timeline and cost, and the experience to recognize risks and mitigate them as appropriate when they appear during the transition. In some cases, the transferring site might be different from that of the originator of the process. The process may have been licensed from a hospital, an academic institution, or another company. Alternatively, the process may require transfer from one CDMO to another. The experience and knowledge of the process originator is fundamental and foundational to success and should be leveraged during a transition.
Transfer of patient-specific therapies can be complicated by the variable nature of starting raw materials. Unlike off-the-shelf processes (in which a master cell bank serves as a consistent and well-defined starting material with patient-specific therapies), starting materials can vary dramatically from patient to patient depending on severity and/or type of illness, age, and differences in cell population percentages. Furthermore, in many situations, material from healthy individuals is used for process development as well as training, engineering, and qualification runs. That material may not represent the variability seen in the affected patient population.
Adding to that complexity is the fact that transfer of patient-specific therapies separates the clinical site (and patients) from the manufacturing site. Consider the scenario outlined in Figure 1, in which a therapeutic product is developed at an academic medical center. Before technology transfer, collection of biological raw material through apheresis, for example, and manufacturing of the therapeutic product takes place within close physical proximity. Once the process is transferred to a CDMO, collection of starting materials and manufacture of the therapeutic product are separated by time and distance. In such cases, it is critical to establish that starting materials (e.g., apheresis product) will retain key quality characteristics during shipment and will remain stable during shipment from collection site to manufacturing site.
Partnering with an experienced CDMO allows the transferring site to identify and overcome those and other challenges and use specific services and capacity as required by project timelines and fiscal and fundraising constraints. A CDMO also can facilitate process integration and execute seamless transitions through technology transfer stage checkpoints as well as incorporate key analytical method-development goals.
Application of a systematic approach during such a critical transition can help ensure timely progress toward — and achievement of — milestones. Once the decision has been made to execute a technology transfer, a number of factors can combine to determine the success of the engagement.
Set the Strategy
The first step toward a successful technology transfer must be a clear, well-defined strategy that addresses scope, timeline, and resources at both the transferring and receiving site. It should be agreed upon by all stakeholders and defined consistently with the clinical development plan.
Describe the processes that will be transferred: They will include (but are not limited to) the receipt and accession of the starting material at the receiving site, manufacture of the cell therapy product, in-process and final product testing using analytical methods, product release and shipment of final product to the clinical site, and other ancillary processes that are required to successfully complete the clinical manufacturing process. Include a detailed description of processes being transferred for specific technologies, and define process parameters and set expectations for those processes. The process description also should describe possible process or equipment adaptations of the receiving site compared with the transferring site.
Describe the analytical methods being transferred: These can include (but are not limited to) tests performed on incoming product raw material (e.g., apheresis) in-process samples, identity and potency assays, and final product testing (e.g., cell counts, viability determination, phenotype, endotoxin, sterility, and mycoplasma testing). Include a description of the analytical methods that are for specific testing technologies.
Documentation: In your transfer strategy, include a gap analysis and risk assessment of the process and analytical methods being transferred. Also include a quality agreement to align the expectations for quality assurance between the organizations. The agreement should detail the requirements for qualification studies and the process for handling process deviations. In addition, assess the need for a comparability study using material generated during the technology transfer, before or during process qualification (PQ) runs.
Other Aspects: The transfer strategy should also detail
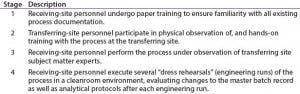
Table 1: Four stages of training at the transferring and receiving sites
• onsite training of receiving-site personnel first at the transferring site before transfer and again at the receiving site (Table 1), with mutually agreed-upon criteria to assess the effectiveness of the training
• practice runs performed by trained staff at the receiving site to assess the technology transfer and compare it to the original success criteria determined at project onset
• the number of technical transfer batches that will be produced and at what scale (Table 2)
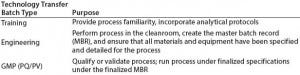
Table 2: Types of batches prepared during the technology transfer process
• analytical methods qualification and acceptance criteria
• the number of engineering runs and acceptance criteria.
Your engineering run definition should include processes performed at full-scale in a cleanroom. That allows for completion of a master batch record (MBR), verification of analytic methods, and completion of all raw material and supply logistics (including shipment of the final product and assessment of the technology transfer against predefined acceptance criteria). The engineering run definition may or may not include full quality review and release.
Finally, the transfer strategy should describe the number of PQ or verification runs and acceptance criteria. Processes must be performed under full current good manufacturing practice (CGMP), with the finalized and approved MBR and ancillary standard operating procedures (SOPs) in the clinical manufacturing facility. Conduct full testing using qualified analytical methods and regulatory-compliant final product release and shipment.
Time the Transfer
Technology transfer relocates a process into a different environment. As a result, the transfer process should be properly defined before a move is initiated. The time is right for a technology transfer when ranges for quality, final product, and in-process parameters are well understood and robust.
The transfer must include information about parameters before and after individual unit operations as well as ranges for expected recoveries and/or yields across unit operations. Critical process parameters (CPPs) must be evaluated on the basis of historical data, and CPPs with potentially high impact on critical quality attributes (CQAs) must be identified. Technical operations experts on the transferring team evaluate CPPs and CQAs, so information from processes that failed or did not proceed as expected during development can provide extremely useful information. The transferring company also must define acceptance criteria for incoming raw materials (e.g., apheresis), other biological materials used in a process, and critical process steps. The final cell-therapy product should be defined and ranges established based on data collected during process development and maturation.
Identify Milestones
The transferring site should identify key development and clinical milestones and come to agreement with the receiving site on necessary and practical timelines. Technology transfer must be built into the overall timeline for product development and commercialization. Often, external deadlines — such as a desired investigational new drug (IND) submission date or funding milestones — can drive the timelines of technology transfer, but care must be taken to allow both parties sufficient time to successfully proceed through transfer stages. Technology transfer is a marathon, not a sprint.
Sharing Information
Open and honest sharing of information from sponsor to CDMO is critical for success. Process descriptions, protocols, SOPs, work instructions (WIs), and MBR (if already developed by the transferring site) all contain useful information for performing a given process. However, technology transfer teams should not underestimate the criticality of unspoken and unwritten information inherent to scientists, operators, and technicians at a CDMO. The originating facility, if different from the transferring site, should be involved to ensure capture of the full history of a process.
To develop a technical understanding of the technology to be transferred, a combined team (with members from both sponsor and CDMO) should review all available scientific and technical data and documentation. Those materials should include process development reports, a process description, SOPs, material and equipment specifications, acceptance criteria, logistics, and clinical considerations.
The CDMO also must understand biological material and final product variability, process consistency and robustness, and failure rates. The CDMO should leverage experience gained through previous technology transfers to preempt and mitigate potential risks to the success of the project.
Once the receiving site has reviewed all provided information, additional development activities might be required. Such activities should be performed after technology transfer and under strict change control.
Program Kickoff and Charter
After agreements have been made to move forward with a collaborative project, a project initiation meeting is the first major milestone in technology transfer. During that meeting, expert team members from both the transferring and receiving sites meet, transfer technical and logistic information, and lay the groundwork for a program charter. Next comes a program kickoff meeting at the CDMO site to detail the basic science, manufacturing process, analytical and testing procedures, storage, shipping, and all other technical issues specific to the project.
A program charter is a high-level document developed and agreed upon by all team members. It lays the groundwork for a program and captures all important elements in a format that is readily understandable by all members of the team implementing the program. This provides a central point of reference and formal agreement of program scope, deliverables, and constraints. Specifically, a program charter should identify the following:
• Stakeholders (roles, responsibilities, communication plan)
• Technology transfer strategy (the transfer activities, need for process development or improvements once transfer has been completed, training, process implementation, and process qualification)
• Timeline
• Assumptions
• Risk assessments and gap analyses.
Define Roles and Responsibilities, and Set Up Communication Paths
Upon establishing a collaborative sponsor–CDMO team, it is crucial to set expectations for open communication between both parties. A communication plan compiled jointly will identify the roles and responsibilities of team members at the sponsor and/or transferring site and the CDMO, summarize expectations, and provide an up‑to‑date and comprehensive list of contact information available to the team. This document should be revisited and updated regularly as a project moves between stages.
Successful technology transfer occurs when team members on all sides of the transfer develop an open and proactive relationship with their counterparts, enabling frequent and timely communication as matters arise. To eliminate redundancy and duplication of effort, important information, decisions, and discussion summaries must be circulated to the extended team.
Team members should be proactive, take ownership of individual roles, and maintain accountability. Internal team communications also should not be overlooked, because consistent messaging between the transferring and receiving site will reduce confusion and frustration for all. A central and secure location (such as the Microsoft SharePoint online hosting service) to house all project‑related documentation is essential to ensure that everyone has access to the same information at any given time. Additionally, staff turnover happens at both the transferring and receiving sites. So a central point of reference and open team-wide sharing of information can help mitigate loss of information caused by such turnovers.
Part two of this article will discuss critical success factors, best practices, and key strategies that will facilitate the successful transfer of a cell therapy manufacturing process.
Reference
1 Mackay, G. State of the Regenerative Medicine Industry. Alliance for Regenerative Medicine Annual Meeting 2014, 13 January 2014; http://alliancerm.org/sites/default/files/ ARM_SOTI_PPT_2014.pdf. •
Catherine McIntyre, PhD, is director of technical operations at PCT West, 291 N. Bernardo Avenue, Mountain View, CA 94043. Cenk Sumen, PhD, is manager of technology and business development at Progenitor Cell Therapy, 4 Pearl Court Suite C, Allendale, NJ 07401; 1-201-312-0840; [email protected].
You May Also Like





