Quality by Design: Current Regulatory Status and Future Challenges
Drug manufacturers face the very real challenge of being both innovative and efficient — having to get products to market quickly — whilst at the same time facing existing hurdles that can limit both of these goals. To manufacture products innovatively and quickly, while at the same time reducing costs and ensuring quality, drug manufacturers must find ways to build quality into their processes. Doing so will aid in product approvals, cut down on poor design issues and ultimately lead to a reduction in costs as, currently, quality assessments rely heavily on end-product testing. The pharmaceutical industry and regulators understand the need to move from end-product testing to a more enhanced quality model. The ideal model would utilize the concepts of quality by design, risk management and quality systems for identification, prioritization, design and product quality control. The focus should now be on how to overcome the hurdles to implementing these key concepts.
Traditional Pharma
Compared with many industries, the pharmaceutical industry does not routinely utilize enhanced quality systems and state-of-the art equipment. Drug manufacturing processes have been in existence for decades, a few for more than a century, a few for over a century and, in many cases, the ageing facilities and equipment in use then are still in use now. Processes that were quickly developed and submitted to regulatory authorities decades ago remain virtually unchanged. These processes, while delivering acceptable product, also have high reject rates and production costs when compared with other industries. The pharmaceutical industry would benefit from continually modernizing processes using quality concepts and new technology that enhance throughput and provide improved quality and control.
There are many factors that have led to this ‘traditional’ state of pharmaceutical manufacturing. It begins with the focus on drug development, continues to concentrate on the clinical aspects of showing adequate safety and efficacy, and delays most efforts for quality by design until the clinical case has been proven. Although this is financially prudent, it results in a race to register a product with limited understanding and optimization of the manufacturing and testing schemes. Delays in getting products approved result in “lost opportunities” for the firm because there is a limited lifecycle for a pharmaceutical product to return the development investment as patents run out and generic competition drives significant decreases in revenue. The result of launching with a suboptimal process leads manufacturers to reject product batches because of issues that could have been avoided by placing more emphasis on understanding and controlling the processing during the development cycle of the drug. Some manufacturers face inefficient or poorly designed processes that result in extremely high waste, which dramatically lowers yields. This is a direct result of the inability of the manufacturer to predict or fully understand their processes and the reasons for these failures.
Traditionally, the way scale-up is approached organizationally is a major contributor to the problem. Most drug manufacturers have highly skilled personnel with process development backgrounds working on the upstream and downstream drug development process. Phase I, II and III clinical programmes can be supplied by small-scale processes that do not focus on understanding the constraints of the process, which may lead to failure and rejection. In addition, the personnel that are responsible for the scale-up activity may not have been directly involved with the development of the small-scale process, and they have limited time to perform the transfer and hand the full-scale process over to the production facility. Often, there is inefficient interaction between the personnel that develop and scale-up the process and those that are responsible for commercial production. This results in a limited knowledge transfer and processes being forced into the production facility to meet submission and launch timelines. This leads to the discovery of critical quality attributes and critical process controls the hard way — when a clinical process is handed off to manufacturing and disasters happen. At this late stage, it is far more expensive to discover that certain controls are lacking, product is wasted in alarming and expensive amounts or, worse yet, that regulatory challenges have arisen that require extensive evaluation and consideration prior to implementation. Marketing plans have been drawn and, subsequently, distribution dates have been anticipated. Project Managers are reluctant to entertain the possibility of changes at this point, and upper management has already been anticipating the impact to revenue streams. Change under these conditions is extremely unpopular and, thus, only mission critical changes are made. Most optimization issues are delayed until after launch and handled as post-approval changes.

In addition to the drug development practices and organizational issues already mentioned, the Good Manufacturing Practice (GMP) requirements themselves are seen as supporting the traditional end-product testing paradigm to ensure product quality. The GMPs do not address product development in the same way that Device GMPs do. Even global regulatory submission formats do not address how critical quality attributes were identified and the development of an overall control strategy through process understanding and knowledge.
The Desired State
In various presentations to industry leaders, FDA’s Director of the Center of Drug Evaluation and Research (CDER), Janet Woodcock, described this desired state as “a maximally efficient, agile, flexible pharmaceutical manufacturing sector that reliably produces high-quality drug products without extensive regulatory oversight.” This vision is shared by industry and regulators alike. The challenge is how do we get to this desired state?
Because quality by design, risk management and quality systems are being introduced as new concepts and ways to do business, it is extremely important to establish common terms and definitions to facilitate the discussion and evolution of these concepts. International Conference on Harmonization (ICH) documents provide global definitions and descriptions of key quality concepts to be adopted. The ICH has tackled the topics of Pharmaceutical Development, Risk Management and Pharmaceutical Quality Systems as Q8, Q9 and Q10. These have been developed and approved through the ICH process. Q8 (Pharmaceutical Development) has just had its first revision approved and focuses on quality by design guidance for pharmaceutical drug products. The establishment of Q8, 9 and 10 provides guidance on the concepts of Pharmaceutical Development, Risk Management and Quality Systems, but are not “how to” documents. Firms must determine how to best integrate these concepts into their company specific programmes and processes. There are a number of key questions and concerns that industry and regulators are working on to evolve the maturity of these concepts into more practical guidance:
First and foremost, quantifying the benefits of a QbD approach today and at some future point where “regulatory flexibility” may be achieved.
What amount of regulator oversight is needed to take advantage of a QbD approach? For instance, how much information and knowledge should a firm provide in a regulatory submission to describe the design space and control strategy?
Questions remain regarding the regulatory inspection approach to review risk assessments that firms may perform as a part of a QbD
Risk Management programme. Although the Q8, 9 and 10 concepts are not strictly required by global regulations, they are becoming expectations, and many firms have begun implementing these concepts because of their business benefits. Once these programs are described in GMP procedures as systems, they become open to inspections. It is not clear how these will be used to assess the adequacy of the quality unit and compliance with GMPs. The implementation of QbD brings with it a host of questions that a firm will ask itself to determine whether or not to implement and, if so, to what extent. For example
What are the costs and what is the likely return on that investment (fewer rejected batches, less scrap, less rework, etc.)?
Will there be some type of “regulatory flexibility” for those firms that adopt QbD and adequately identify their critical quality attributes, understand their process and develop a robust control strategy that ensures proper quality of the drug product?
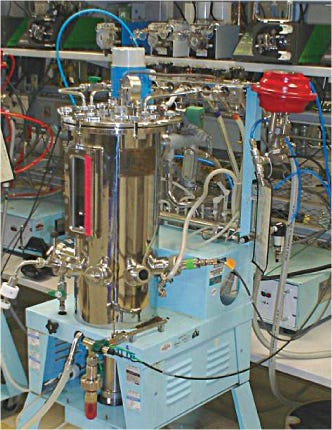
Process development lab bioreactor at Amgen

60 L bioreactor at Amgen
Because of the nature of pharmaceutical development, many firms find themselves waiting until proof-of-concept before performing any real process assessment. Even after passing the proof-of-concept hurdle, firms may limit process optimization until the product has passed the efficacy and safety hurdles. This may result in the need to submit a more traditional filing to regulatory authorities and modify this file with more complete process knowledge and control strategy after approval. What will be the mechanisms for a post approval adoption of a QbD approach?
ICH has taken on a new topic, Q11, “Development and Manufacturing of the Drug Substance.” This topic will bridge the QbD concepts of Q8 Drug Product (DP) to Drug Substance (DS), along with addressing the lifecycle management of the manufacturing process. This topic has a number of issues to address, including difference of QbD for DP versus DS, small molecule versus large molecule and traditional versus enhanced approach.
When fully considered and implemented, Quality by Design translates to better-developed critical quality attributes for drug product, drug substance and raw materials. In addition, all critical sources of process variability have been identified in a control strategy, measures have been taken and controls have been put in place to mitigate unacceptable risks. The benefits of this include the following:
Product waste is minimal
Fewer process controls are required or the existing controls are more meaningful
Batch cycle times are minimize
The impact of process changes are fully understood
Costly equipment and processing changes are limited
Faster/more successful regulatory approval
Project deadlines are on target
Marketing dates and subsequent revenue streams are hit
Utilization of enhanced manufacturing approaches that allows manufacturers to vary the process based on variable inputs to produce more consistent drug product.
Where Do We Go from Here?
One of the most fundamental issues that drug manufacturers are facing is how to manage the development and transfer of new drugs to existing, and in some cases, outdated or inefficient manufacturing processes. It is cost-prohibitive to build new facilities for every new drug that is planned. Likewise, it is extremely time consuming and expensive to retrofit or radically alter existing facilities and processes for each new drug. In some cases, it is a monumental task to apply principles of QbD to these existing caveats. Many manufacturers struggle with concepts such as QbD because they simply face the overwhelming task of implementing these programmes into existing processes.
It would benefit the industry to examine new technology to meet this challenge, but new technology carries with it similar hurdles. Additional challenges that the industry faces in implementing the principles of QbD include the following:
How to handle existing products compared with new products approved with QbD principles
Determining how a QbD approach can be optimized, given the nature of pharmaceutical development and the potential for clinical failure late into the programme.
How can the principles of QbD be applied to complex molecules that have multiple variables that need to be controlled for each unit operation?
Are there optimal organizational structures that enhance and facilitate the adoption of QbD principles, particularly the hand-off from development to manufacturing?
Conclusion
We are embarking on a journey to develop enhanced quality principles for pharmaceutical manufacturing. There are differences between industry and regulatory agencies around the globe regarding the interpretation of QbD principles. Work by ICH is important to define key terms and concepts, to facilitate further dialog between industry and regulatory authorities and bring both business and regulatory rewards to those that adopt QbD approach. While it should be somewhat easier to apply these principles to new drug products and processes, there is a need to bridge the gap to include the introduction of QbD to existing systems. This is an exciting time for the pharmaceutical manufacturing industry as these principles are applied in the ongoing effort to ensure a more consistent quality product.
The views expressed herein represent those of the authors and do not necessarily represent the views or practices of the authors’ employer or any other party.
You May Also Like





