Voices of Biotech
Podcast: MilliporeSigma says education vital to creating unbreakable chain for sustainability
MilliporeSigma discusses the importance of people, education, and the benefits of embracing discomfort to bolster sustainability efforts.
April 1, 2013
Polymerases are natural enzymes that are vital to nucleic acid synthesis: DNA polymerase for replication of deoxyribonucleic acid and RNA polymerase for replication of ribonucleic acid. Thus all living things make and use polymerases of their own. But in 1969, the University of Wisconsin’s Thomas D. Brock and Hudson Freeze identified a new species of extremophilic bacterium thriving at 160 °F (70 °C) in a hot spring in Yellowstone National Park. In time, heat-tolerant polymerase isolated from Thermus aquaticus (Taq) would lead to an amazingly simple laboratory technique with hundreds of valuable uses in molecular biology: the polymerase chain reaction (PCR).

PCR uses in vitro enzymatic synthesis to amplify specific DNA sequences, producing as much as 100 billion copies of a single molecule in just a few hours. It has “revolutionized research in the biological sciences and medicine, and has influenced criminology and law” (1). The technique finds utility in many aspects of biological research. It is also used by criminologists to link specific persons to samples of blood or hair. PCR has helped evolutionary biologists by enabling large quantities of DNA to be made from ancient remains containing trace amounts (2).
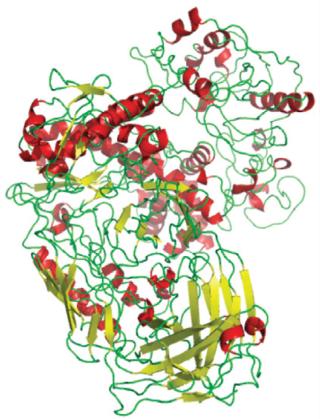
How It Works: Thanks to thermal cyclers from companies such as Bibby Scientific/Techne, Cole-Parmer, Eppendorf, and many others listed below, a scientist’s part in the PCR procedure is little more than “add reagents and stir,” although the chemistry involved is impressive. First drop a little bit of DNA into a test tube and add a large sample of loose nucleotides. Then add a pair of synthesized short DNA segments that match both ends of your gene of interest. When those “primers” run into the right DNA sequence, they provide starting points for copying. The Taq polymerase (Figure 1) locks some nucleotides into a sequence dictated by that target gene. When you heat your sample, the DNA double helix separates into two strands. Each exposed primer bases automatically bind to complementary portions bases in the sample as it cools. And the enzyme links more loose nucleotides to the primers and separated DNA strands with the specified sequence. The whole reaction takes about five minutes, creating two double helices where before there was one. This heating–cooling cycle then repeats, doubling the number of DNA copies each time. After 30–40 cycles, a single sequence is “amplified” to hundreds of millions of copies (2).
As a lay person, I was amazed to successfully perform just such a procedure myself in a “biotech for journalists” laboratory course some years ago. It’s that easy. Kits and instruments from laboratory vendors such as Agilent Technologies, Bio-Rad Laboratories, Clontech Laboratories, Illumina Inc., Life Technologies, PE Biosystems, Promega Corporation, Qiagen, Sigma-Aldrich Company, and Thermo Scientific make it even more straightforward. Modern thermal cyclers accommodate many samples, have precise thermal profiles, and are programmable (3).
A Brief History
As with other valuable analytical techniques, decades of major scientific discoveries were essential for development of PCR technology: from Watson, Crick, and Carter’s elucidation of the DNA double helix and Arthur Kornberg’s discovery of polymerases involved in its replication in the 1950s… through H. Gobind Khorana’s work on the genetic code in the 1960s… to DNA repair synthesis work in his laboratory and Frederick Sanger’s sequencing in the 1970s. Nobel prizes came from many of those efforts. But the value of engineering should never be underestimated: Without the thermal cycler, PCR would never have come so far.
Working as a chemist for Cetus Corporation, one of the first biotechnology companies, Kary B. Mullis invented the basic technique in 1985. His manual PCR technique was slow and labor-intensive, so Henry Erlich, David Gelfand, and other colleagues at Cetus soon began looking for ways to automate the process (4). And that’s where the thermostable Taq enzyme comes in. Using other polymerases, a scientist had to add fresh enzyme to each cycle because it would be destroyed by the heat. And Cetus engineers had addressed that need with the first thermocycling machine. But the Taq polymerase allows an instrument to cycle more rapidly without pausing for addition of more polymerase. A 1985 joint venture between Cetus and Perkin-Elmer led to the DNA thermal cycler instruments we know today (2).
Another underappreciated contribution came with development of reliable automated technologies for oligonucleotide synthesis. “Until recently, the construction of a single oligonucleotide was a substantial task that could only be performed by a skilled organic chemist. Now it is possible to purchase either an oligonucleotide synthesizer that can be operated by a technician or the oligonucleotides themselves from a commercial or academic source” (3). Such instruments and related custom oligo services from Azco Biotech, Bio-Synthesis Inc., GE Healthcare, Integrated DNA Technologies, and many of the companies listed above have greatly reduced the cost of oligos, which define the products of PCR. Without a ready supply of them, it “would not have enjoyed the wide acceptance that it has gained today” (3).
By 1988, Cetus was inundated with licensing inquiries: Companies wanted to use PCR for commercial diagnostics. So in 1989, Cetus collaborated with F. Hoffmann-La Roche on commercialization of in vitro diagnostic products and services based on PCR (2). Roche Molecular Systems eventually bought the PCR patent and associated technology from Cetus for US$300 million in 1991 (2). That investment paid off as the company launched many related products and services from it (4).
Modern PCR techniques and instruments amplify DNA fragments up to several kilobases in length (3). Although PCR is the most widely used method for in vitro amplification, the thermal denaturation of DNA strands has proven to be a limitation. Sequence mistakes can and do result — and they get amplified too. DNA replicates naturally by polymerases using accessory proteins such as DNA helicase, which separates double
-stranded DNA inside cells. A relatively new method called helicase-dependent amplification (HDA) mimics that in vivo process by using the enzyme to generate single-stranded templates for primer hybridization without Taq(3). By eliminating thermal cyclers and allowing for isothermal amplification, HDA facilitates the PCR process.
Applications
As PCR was put into practice over the years, many other variations on the theme emerged. Different types of laboratories have different needs, and sometimes small modifications can fill those needs. For example, multiplex PCR used for “DNA fingerprinting” simply uses more than one primer for simultaneous analysis of multiple targets in a single sample. Other variations involve pretreatment or combining PCR with other technologies, adjusting its components to optimize performance, modifying primers or using other polymerases, or turning the technique upside down by amplifying unknown sequences that surround a known sequence (inverse PCR).
Dozens of variations have been developed, but the one that’s most familiar to biopharmaceutical development laboratories is the highly precise quantitative PCR (Q-PCR) method. It measures the amount of a specific sequence initially present in a sample by mathematical extrapolation back from the results of exponential amplification. Special thermal cyclers are required to monitor those results as a reaction progresses. And quantitative real-time PCR methods — QRT-PCR, not to be confused with reverse-transcriptase PCR (RT-PCR) — involve a broad array of fluorescent dyes and fluorophore-containing DNA probes to help do so.
Diagnostic Q-PCR is applied to rapidly detect nucleic acids that indicate the presence of infectious diseases, cancer, and genetic abnormalities — making it vital to product development in those areas and to personalized medicine in general (5). It is also used to detect emerging diseases, such as new strains of influenza. QRT-PCR can measure gene transcription, as in cell line development. It can help scientists determine how expression of a particular gene changes over time — in preclinical studies as well as genetic stability testing of cell lines, in differentiation studies of stem cells, and in transgenic plant or animal development. RT-PCR provides qualitative information of gene expression (rather than quantitative) and focuses on RNA rather than DNA, but it finds use in many of the same laboratories and similar studies. PCR is also a powerful tool for contamination detection, identification, and monitoring/control of bacteria, viruses, and host-cell residuals (6, 7). It is limited only by the numbers and types of oligonucleotide primers available (8, 9).
Optimization of PCR processes involves determining the accuracy of those primers and finding their ideal concentration in solution, trying different reaction times and temperatures, and in the case of multiplex assay development, performing separate tests (“singleplex assays”) for each set of primers involved (10). In troubleshooting their results, scientists often find that sample contamination can foul the whole process. And inhibitor molecules may get in the way. So good sample preparation is very important, as is proper maintenance of equipment and instruments between PCR runs. Some primers may dimerize, making them unavailable for the reaction; usually the solution to that problem is simply adding more of them. As the “Vendor Expertise” box shows, several suppliers of PCR kits, reagents, and instruments have published excellent guides on these topics.
One challenge with Q-PCR assays comes in determining the exact point at which to measure and calculate the results. PCR amplification goes through an exponential phase of copying, but that is limited by reagent availability in the sample, so it’s not always easy to tell when that phase comes to an end. If you do the math using the wrong variables (that is, measuring at the wrong time), then the results can be misleading. Competitive PCR compensates for this problem by normalizing the end-product based on a ratio between target and competitor sequences. The method has been described as cumbersome, however, because it requires a carefully constructed competitor target for each reaction and a series of dilutions to ensure the correct ratio. QRT-PCR was developed as an alternative solution.
Finally, it is worth noting that the Human Genome Project and corresponding commercial sequencing efforts led by Celera Genomics would not have been possible without PCR (11). Studies of single-nucleotide polymorphisms (SNPs) associated with various diseases would be particularly difficult without PCR to generate enough DNA for research.
PCR from the BPI Archives at www.bioprocessintl.com
Xu Y, et al. Mycoplasma In-Process and Lot-Release Testing: To PCR or Not to PCR (Proceedings of the WCBP CMC Strategy Forum, 19 September 2003) BioProcess Int. 3(11) 2005: 30–39.
Whitford W, Julien C. Appendix 1: Designing for Process Robustness. BioProcess Int. 6(3) 2008: S34–S44.
Robinson CJ, Little LE, Wallny H-J. Bioassay Survey 2006–2007. BioProcess Int. 6(3) 2008: 38–48.
Akers JA, Meltzer TH, Jornitz MW. The Reoccurrence of Mycoplasma Contamination: Prevention Strategies. BioProcess Int. 7(2) 2009: S44–S47.
Kuhlman PA, et al. Rapid Purification of Lys-C from Lysobacter enzymogenes Cultures. BioProcess Int. 7(2) 2009: 28–38.
Brown DB, et al. Assay Validation for Rapid Detection of Mycoplasma Contamination. BioProcess Int. 7(4) 2009: 30–40.
Schirmer EB, et al. Primary Clarification of Very High-Density Cell Culture Harvests By Enhanced Cell Settling. BioProcess Int. 8(1) 2010: 32–39.
Fike R. Nutrient Supplementation Strategies for Biopharmaceutical Production, Part 3. BioProcess Int. 8(1) 2010: 24–31.
Tsuji S, et al. An Efficient Thermoinducible Bacterial Suicide System. BioProcess Int. 8(4) 2010: 28–40.
Liu X, et al. Isolation of Novel High-Osmolarity Resistant CHO DG44 Cells After Suspension of DNA Mismatch Repair. BioProcess Int. 8(4) 2010: 68–76.
Hitchcock AG, et al. Scale-Up of a Plasmid DNA Purification Process. BioProcess Int. 8(11) 2010: 46–54.
Filipe V, Jiskoot W, Hawe A. Understanding Virus Preparations Using Nanoscale Particle Characterization. BioProcess Int. 9(2) 2011: 44–51.
Monesmith TT. Meeting the Challenges in Manufacturing Autologous Cellular Therapies. BioProcess Int. 9(3) 2011: S38–S41.
Adams G, et al. Trends and New Technology in Vaccine Manufacturing. BioProcess Int. 9(8) 2011: S28–S35.
Stepp PC, et al. Comparing H1N1 Virus Quantification with a Unique Flow Cytometer and Quantitative PCR. BioProcess Int. 9(8) 2011: S50–S56.
Langer ES. Limited Analytical Technologies Are Inhibiting Industry Growth. BioProcess Int. 9(9) 2011: 18–23.
Menendez AT, et al. Recommendations for Cell Banks Used in GXP Assays. BioProcess Int. 10(1) 2012: 26–40.
Liu N, et al. Host Cellular Protein Quantification. BioProcess Int. 10(2) 2012: 44–50.
Vaes B, Craeye D, Pinxteren J. Quality Control During Manufacture of a Stem Cell Therapeutic. BioProcess Int. 10(3) 2012: 50–55.
Aranha H. Current Issues in Assuring Virological Safety of Biopharmaceuticals. BioProcess Int. 10(3) 2012: 12–17.
Brooks A, Davis A. Advancements in Processing That Optimize Samples for Future Research. BioProcess Int. 10(8) 2012: 62–69.
Jordan I, et al. Production of a Viral-Vectored Vaccine Candidat
e Against Tuberculosis. BioProcess Int. 10(8) 2012: 46–55.
Thompson AS. Rapid Detection of Pandemics. BioProcess Int. 11(1) 2013: 60.
Getting Together
If your laboratory is lacking in PCR skills and equipment, you can always engage the expertise of a service provider such as Benten Bioservices, BioReliance, or Charles River Laboratories. “At Benten BioServices,” says president and CEO Paula Z. MacDonald, “we apply PCR technology in support of process development activities, regulatory filings, and product lot release. The methodology is particularly useful for the fast time to achieve results, acceptance by global regulatory agencies, and applicability to some infectious agents that are noncultivable. We develop and validate assays to detect and quantify contaminants, such as mycoplasmas, viruses, yeasts, bacteria and residual DNA and RNA from bioprocesses using Q-PCR.”
But if you just need to brush up on the latest developments, you’ll have to dig into the technical programs of several upcoming life-science conferences — such as IBC Life Sciences’ “Biological Assays” meeting (mid-May in Seattle, WA), “Cell Line Development and Engineering” conference (San Diego, CA, also in May), and “Applications for Enzyme Technologies” event (San Francisco, CA, in June), as well as “BioProcess International China” (August in Shanghai) and of course the “BioProcess International Conference and Exhibition” (September in Boston, MA).
I couldn’t find many events that focus on PCR specifically. There was the inaugural “Quantitative Real-Time PCR: Applications for Molecular Diagnostics” symposium in San Francisco this past February — part of Molecular Med’s Tri-Con 2013 event. We hope to see a similar program repeated in the future.
An event we do expect to see again was held at the Technical University of Munich in Germany this past March. The sixth international “Next Generation Thinking in Molecular Diagnostics” symposium and industrial exhibition included talks and application workshops focused on qPCR and next-generation sequencing technologies. Keep your eye on www.qpcr-ngs-2013.net for information about the next installment.
This October in San Diego, CA, Cambridge Healthtech Institute is producing its second annual meeting that focuses on “Digital PCR Technology and Tools for Precision Diagnostics.” CHI says that dPCR is “a single-molecule counting method that quantitatively measures absolute DNA and eliminates the need for standard curves” and that it could be a disruptive technology for diagnostics. This event will bring together industry visionaries and early adopters to discuss its capabilities, limitations, and future applications. Devices from start-up companies and academic laboratories will be showcased. Topics to be addressed include integrating dPCR with other technologies, solutions for processing difficult samples and increasing throughput, and guidelines and best practices for digital detection.
Also in October, the historic Kurhaus, famous for its seaside location close to The Hague, will host the eighth “European Meeting on Molecular Diagnostics” in Scheveningen, The Netherlands. Devoted to all aspects of molecular diagnostics in human disease and pathology, EMMD will focus on novel molecular technologies and their innovative applications in disease diagnosis, monitoring, and screening.
Vendor Expertise
Agilent Technologies:www.genomics.agilent.com/CollectionOverview.aspx?PageType=Application&SubPageType=ApplicationOverview&PageID=291
Eurogentec:www.eurogentec.com/uploads/qPCR-guide.pdf
Illumina:www.illumina.com/applications/real-time-pcr.ilmn
Promega:www.promega.com/products/pcr/qpcr-and-rt-qpcr/
Rapid Test Methods:www.rapidmicrobiology.com/test-methods/Rapid-Method-Pharma.php
Sigma:www.sigmaaldrich.com/life-science/molecular-biology/pcr/quantitative-pcr/qpcr-technical-guide.html
Meanwhile, check out our archives for some previous BPI articles that report on PCR applications. And with hundreds of thousands of scientific papers reporting on its use in a body of literature that’s growing every day, you’re sure to find just the help you need. This is one analytical technique that’s proven itself to be robust, versatile, and facile enough to make it a staple in molecular biology laboratories for decades to come.
About the Author
Author Details
Cheryl Scott is cofounder and senior technical editor of BioProcess International, 1574 Coburg Road #242, Eugene, OR 97401; 1-646-957-8879; [email protected].
1.) Templeton, NS. 1992. The Polymerase Chain Reaction: History, Methods, and Applications. Diagn. Mol. Pathol. 1:58-72.
2.) Henson, PM, and R Kondratus. 1992.RU 9577: The History of PCRSmithsonian Video History Collection, The Smithsonian Institution, Washington.
3.) 2012.History and Development of the Polymerase Chain Reaction (PCR) Molecular Station.
4.) 2011.Timeline of PCR and Roche, Roche Molecular Systems Inc., Pleasanton.
5.) Valigra, L 2011. PCR Gets Personal, Faster. Pharmaceut. Form. Quality:18-21.
6.) Jimenez, L. 2000. Use of PCR Analysis for Sterility Testing in Pharmaceutical Environments. J. Rapid Meth. Automat. Microbiol. 8:11-20.
7.) Ragheb, SM, AS Yassin, and MA Amin. 2012. The Application of Uniplex, Duplex, and Multiplex PCR for the Absence of Specified Microorganism Testing of Pharmaceutical Excipients and Drug Products. PDA J. Pharmaceut. Sci. Technol. 66:307-317.
8.) Walker, NJ 2002. A Technique Whose Time Has Come. Science 296:557-559.
9.) MacKay, IM 2004. Real-Time PCR in the Microbiology Laboratory. CMI 10:190-212.
10.) qPCR Guide, Eurogentec, Seraing.
11.) Gwynne, P, and G. Heebner. 2001. PCR and Cloning: A Technology for the 21st Century. Science www.sciencemag.org/site/products/pcr.xhtml 9.
You May Also Like